CDC’s Flawed Lyme Tracking System
Changes to the CDC’s Lyme case definition add complexity and case undercounting, leading to missed diagnoses and underfunding.
In January 2022, the U.S. Council of State and Territorial Epidemiologists (CSTE) published a revision to its 2017 Lyme disease case definition. This definition will soon be integrated into the physician reporting form used by the Centers for Disease Control (CDC) to classify, count, and track Lyme disease cases consistently across the country.
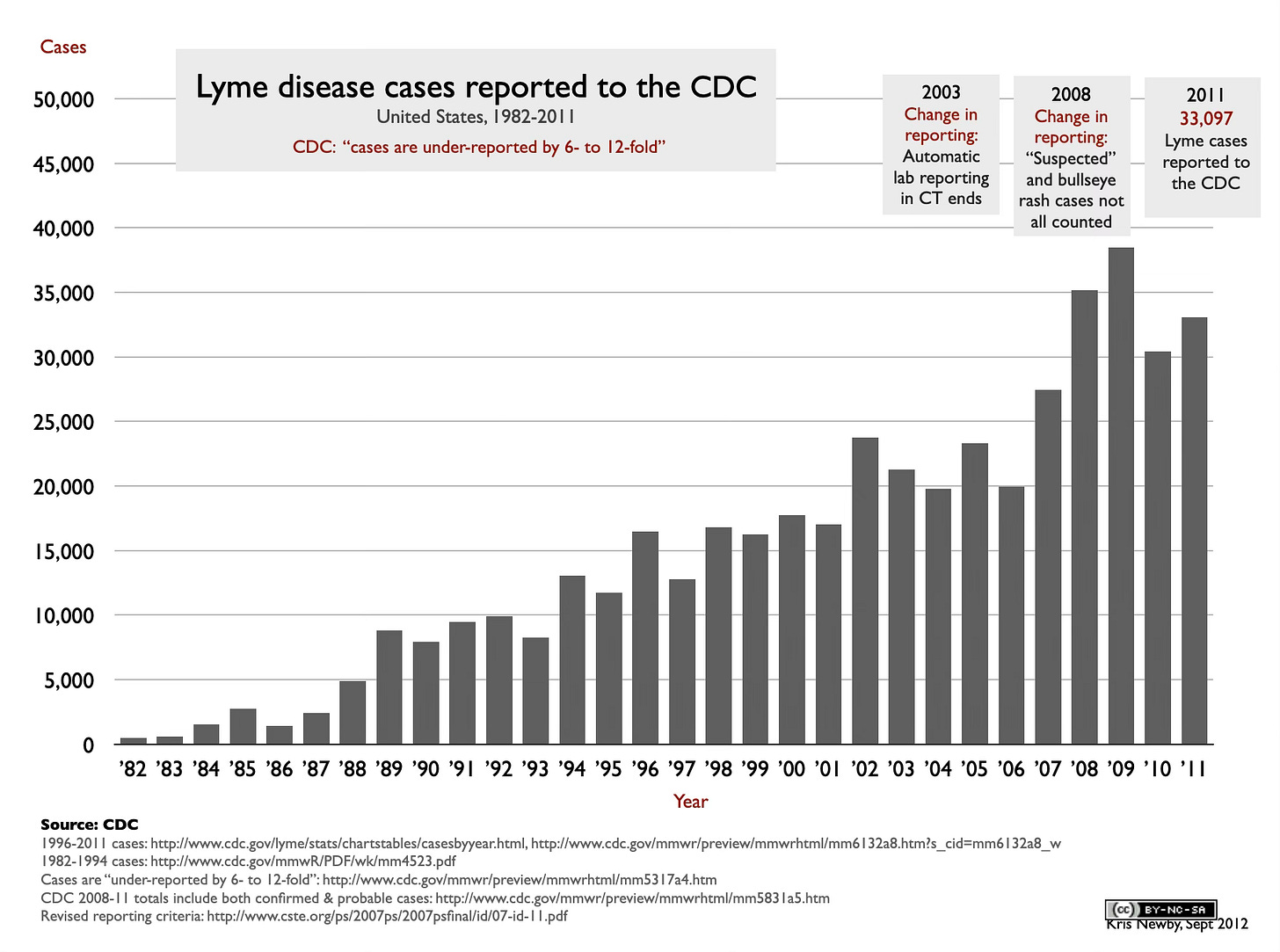
The annual Lyme disease case count is an important metric for allocating government research dollars and staff resources. With about 476,000 new cases a year and growing, the CDC’s previous case definition and reporting requirement was already burdensome for physicians and local health departments. (In 2016, Massachusetts modified the CDC reporting criteria because of this. In 2008, New Jersey wrote about the burdens of the surveillance criteria here.) Unfortunately, the 2022 revision and the public health burden of the COVID-19 pandemic made the situation worse.
The two most significant changes to the definition are the inclusion of Borrelia mayonii, a newly discovered Borrelia burgdorferi family member in the Lyme case count, and the option for physicians to use a cheaper, more straightforward test in the second part of the two-tiered testing protocol. Despite a few positive changes to the 2022 revision, the new definition doesn’t fix some fundamental flaws, which could lead to the undercounting and misdiagnosis of truly ill Lyme patients.
The CDC estimates actual cases may be about ten times higher than reported cases. A 2022 study using insurance claims estimated the annual total to be 476,000.
Here is a summary of significant changes and possible impacts:
Borrelia mayonii cases will be counted…sort of.
Borrelia mayonii is a newly discovered member of the Borrelia burgdorferi sensu lato genospecies that has also been shown to cause Lyme disease. It is primarily found in the upper midwestern United States. Like B. burgdorferi, B. mayonii causes fever, headache, rash, and neck pain in the days after infection and can cause arthritis after a few weeks of illness. It can also cause nausea and vomiting; large, widespread rashes; and a higher concentration of bacteria in the blood than B. burgdorferi. Unfortunately, many of these cases will be overlooked because the traditional Lyme tests only pick up about half the B. mayonii cases, and there are currently no FDA-approved B. mayonii tests on the market. (Mayo clinic, IGeneX, and Medical Diagnostics Lab, among others, offer in-house tests.)
In the two-tiered testing process, the western blot can now be replaced with a cheaper, sometimes less informative, enzyme immunoassay (EIA) test.
Western blots, which display an array of individual antibody bands for both present (IgM) and past (IgG) Lyme infections, are more expensive and more complicated to interpret than EIA tests. But doing away with the western blots eliminates useful clinical data for treating physicians. Some of the antibody protein bands can shed light on neurologic, arthritic, or late-stage manifestations of the disease. In addition, the revision states that only the IgG “late stage” antibody EIA tests need to be used, which doesn’t acknowledge the dormant and relapsing nature of Borrelia infections. The new definition also requires that the EIA tests be FDA-approved, which will discourage the use of accurate, validated in-house tests developed at universities and specialty labs. (FDA approval is only required for tests that are resold to other commercial labs. )
Case reporting has been complicated with geographical requirements that may lead to underreporting.
Two case-reporting decision trees are now required for low- and high-incidence case areas, overlayed with a complex matrix of confirmatory/presumptive evidence and suspect/probable/confirmed classifications. Moreover, determining whether a person lives in a low- or high-incidence area is based on CDC data that’s typically a year or more behind. The complexity of this process will most likely lead to underreporting by our already overloaded healthcare professionals, and it begs the question—is it really necessary? Lyme disease cases have been detected in all 50 states and the District of Columbia, and people are often infected during travel. Why not make reporting simple upfront and let epidemiologists, data from electronic medical records, and advanced informatics software on the backend of the process analyze the disease spread?
On a positive note, the new case definition includes some positive changes. For example, it deemphasized Lyme arthritis symptoms and included other significant symptoms, such as secondary rashes and neurological symptoms like headaches, fatigue, stiff necks, and nerve tingling. Kudos to the CDC for highlighting that the surveillance case definitions are not to be used by healthcare providers to make clinical diagnoses or treatment decisions.
But overall, the fundamental problem with this new case definition is that the CSTE and CDC have added burdensome complexity on top of an already archaic process without trying to streamline it and leverage new data sources and analytical tools to make the case count more accurate.
If there is light at the end of the tunnel, it is that in 2020, the CDC launched a Data Modernization Initiative that may bring more real-time public health data to our decision-makers. We hope that Lyme disease will be included in that system.
Kris Newby is an award-winning medical science writer and the senior producer of the Lyme disease documentary UNDER OUR SKIN. Her book BITTEN: The Secret History of Lyme Disease and Biological Weapons won three international book awards for journalism and narrative nonfiction. Previously, Newby worked for Stanford Medical School, Apple, and other Silicon Valley companies.
If you've found this content useful, please consider supporting it through a small paid subscription. While my posts are free, your paid subscription helps underwrite this independent research. It also helps keep it free for those who cannot afford to pay.
REFERENCES:
CDC’s 2022 Lyme Case Definition:
https://ndc.services.cdc.gov/case-definitions/lyme-disease-2022/
CDC’s 2017 Lyme Case Definition:
https://ndc.services.cdc.gov/case-definitions/lyme-disease-2017/
A comparison of the 2022 and 2017 Lyme case definitions:
https://www.documentcloud.org/documents/22020656-2017-vs-2022-lyme-case-definition
The 2006 CDC Lyme disease case report form:
https://stacks.cdc.gov/view/cdc/44978
FDA approval of EIA tests:
https://www.fda.gov/news-events/press-announcements/fda-clears-new-indications-existing-lyme-disease-tests-may-help-streamline-diagnoses
Effect of electronic laboratory reporting on the burden of Lyme disease surveillance–New Jersey, 2001-2006:
https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5702a4.htm




I got a bullseye rash from a tickbite last summer from weeding a bushy area that is frequented by deer. Urban deer are not only pests but carriers of this disease.
Thank you for writing these articles because while a few tweaks have been made, the epidemiology for Lyme disease remains muddied. Until CDC, NIH make the needed changes as you point out, we will continue to have drastic undercounting.
Keep beating the drums! 🥁